In a 2020 study, geriatricians Murilo Dias and Márlon Aliberti at the University of São Paulo, Brazil, and their colleagues found that one in three people admitted for COVID-19 to a hospital in São Paulo still had at least one symptom a year after they were discharged
4. “That’s a huge problem for the health system,” says Aliberti.
Even so, that problem does not include cases of long COVID that arise after mild SARS-CoV-2 infection. Soares says that most long-COVID studies in Brazil do not address this gap, and it can be particularly hard to do so when few physicians are aware of the condition, how to diagnose it or who might be at particular risk.
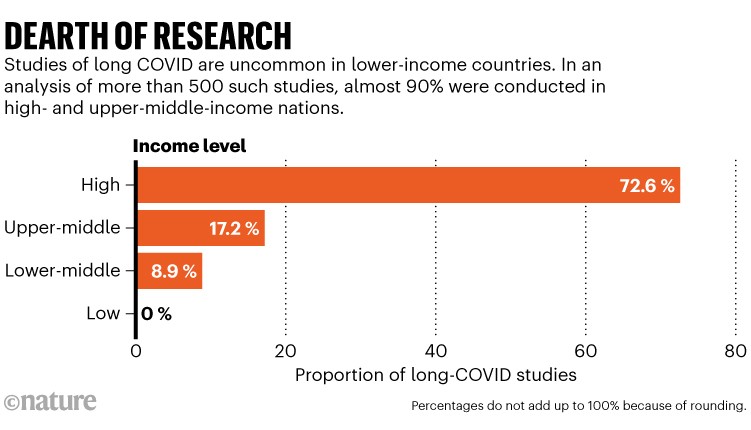
Another reason to study long COVID in different contexts is that the condition might manifest differently from place to place. Many researchers suspect that there are multiple mechanisms underlying long COVID. The risk of the condition might be influenced by genetic and environmental factors, says Olufemi Erinoso, a public-health researcher at the University of Nevada in Reno, who has studied long COVID in Lagos, Nigeria. “We need to have a global approach to the disease to understand how genetics might affect the outcomes.”
Diverse data
To really grasp the mechanism of long COVID, researchers need study participants with diverse genetic backgrounds so that they can work out which cellular pathways are involved and how they might vary in different people. And the more researchers know about those pathways, the more potential targets they’ll have for medicines to treat long COVID. “Not being able to approach the disease in a global, concerted effort is a major impediment to a better understanding and a better therapy for everyone,” says Akiko Iwasaki, an immunologist at Yale University in New Haven, Connecticut.
One trend that looks to be consistent worldwide is that the number of people who develop long COVID seems to be tapering off with the SARS-CoV-2 variants over the past two years. In South Africa, Jassat and her colleagues found a lower incidence of long COVID among those infected with the Omicron variant, compared with the Beta or Delta variants of the virus
3. UK researchers similarly found that Omicron infections were less likely than were Delta infections to lead to long COVID
5. The world has long since moved on from Omicron, but researchers suspect that growing levels of immunity — from vaccination and infection — could also be reducing the number of people at risk of developing long COVID across the globe, says paediatrician Daniel Munblit at Imperial College London, who has studied long COVID in children in Moscow.
This is good news, with one small downside: new studies of long COVID could struggle to recruit participants. This year, Tariro Makadzange, executive director of the research organization Charles River Medical Group in Harare, and her colleagues had trouble including the condition in a study because they found so few fresh cases.
Tailoring treatment
In the United States and Europe, large-scale efforts have begun the search for long-COVID treatments. The US National Institutes of Health is running the US$1.15-billion Researching COVID to Enhance Recovery (RECOVER) programme, some of which is directed at finding long-COVID therapies. In the United Kingdom, a consortium of 30 hospitals and universities is also looking for treatments under the STIMULATE-ICP programme.
But whether any resulting treatments could transfer to lower-income settings is an open question, says infectious-disease specialist Luis Felipe Reyes at the University of La Sabana in Bogotá. He predicts a re-run of the inequalities that plagued the distribution of COVID-19 vaccines. Wealthier countries hoarded doses and some types, such as the mRNA vaccines, were particularly difficult for many lower-income countries to use because they were expensive to produce and difficult to transport at the low temperatures they require.
“The rich countries are finding the treatments for these problems, but those solutions might not be transferable,” Reyes says.
For now, treatments for long COVID often involve careful rehabilitation and, ideally, a collaborative team of specialists in different fields. Such intensive monitoring and care is difficult even for wealthy nations, let alone for countries with more strained health-care systems, says Kimberly Konono, a vaccine specialist at Charles River Medical Group. But even with limited resources, some LMICs have options that are not available in wealthier nations. For example, the public health-care system in Brazil includes a network of community health workers who are embedded in neighbourhoods and often know the occupants well. This network could be used to improve awareness, diagnosis and treatment of long COVID in these regions, says Aveling.
But even that approach relies on health-care systems taking the condition seriously, which hasn’t always happened with some other post-viral illnesses. Similar conditions can follow after other viral infections, including some tropical diseases. These have long been neglected, says anthropologist Jean Segata at the Federal University of Rio Grande do Sul in Porto Alegre, Brazil, particularly when they affect marginalized communities. “Often, these patients complain that they are not taken seriously by doctors, who tell them it’s nothing and that it will pass soon,” he says. “The lack of recognition for their suffering becomes an additional source of frustration and distress for long-COVID patients in impoverished countries.”
Soares, who has been working with Aveling and others to characterize the impact of long COVID in Brazil, can see the effect of this: long COVID and other post-viral illnesses are effectively invisible. “We need to show with data that people are going through these symptoms and the challenge that needs to be addressed,” Soares says. Then she sighs. “I wish that we didn’t have to.”
Nature 625, 20-22 (2024)
doi: Long COVID is a double curse in low-income nations — here’s why[/LEFT][/SIZE]