A blood test for long Covid is possible, new research suggests
Scientists can now show key differences in the blood of those who recover from Covid — and those who don't.
A blood test for long Covid is possible, a study suggests
Scientists can now show key differences in the blood of those who recover from Covid — and those who don't.Sept. 25, 2023, 11:01 AM EDT
By Erika Edwards
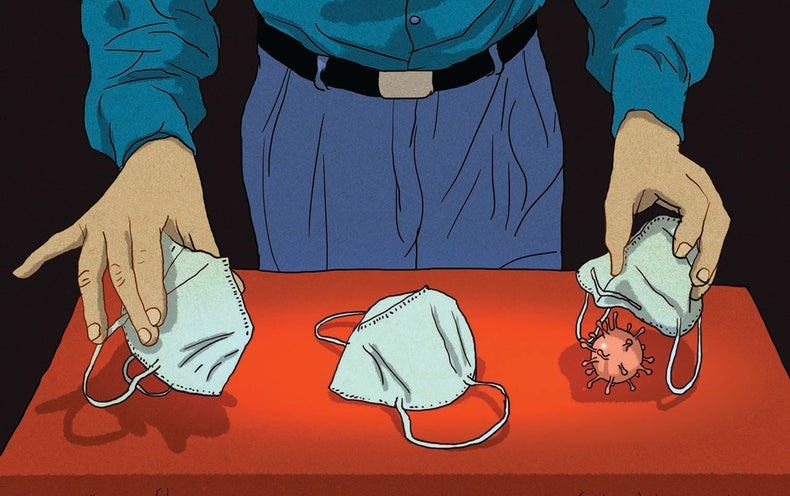
More than three years into the pandemic, the millions of people who have suffered from long Covid finally have scientific proof that their condition is real.
Scientists have found clear differences in the blood of people with long Covid — a key first step in the development of a test to diagnose the illness.
The findings, published Monday in the journal Nature, also offer clues into what could be causing the elusive condition that has perplexed doctors worldwide and left millions with ongoing fatigue, trouble with memory and other debilitating symptoms.
The research is among the first to prove that "long Covid is, in fact, a biological illness," said David Putrino, principal investigator of the new study and a professor of rehabilitation and human performance at the Icahn School of Medicine at Mount Sinai in New York.
Dr. Marc Sala, co-director of the Northwestern Medicine Comprehensive Covid-19 Center in Chicago, called the findings "important." He was not involved with the new research.
"This will need to be investigated with more research, but at least it's something because, quite frankly, right now we don't have any blood tests" either to diagnose long Covid or help doctors understand why it's occurring, he said.
Putrino and his colleagues compared blood samples of 268 people. Some had Covid but had fully recovered, some had never been infected, and the rest had ongoingsymptoms oflong Covid at least four months after their infection.
Several differences in the blood of people with long Covid stood out from the other groups.
The activity of immune system cells called T cells and B cells — which help fight off germs — was "irregular" in long Covid patients, Putrino said. One of the strongest findings, he said, was that long Covid patients tended to have significantly lower levels of a hormone called cortisol.
A major function of the hormone is to make people feel alert and awake. Low cortisol could help explain why many people with long Covid experience profound fatigue, he said.
"It was one of the findings that most definitively separated the folks with long Covid from the people without long Covid," Putrino said.
The finding likely signals that the brain is having trouble regulating hormones. The research team plans to dig deeper into the role cortisol may play in long Covid in future studies.
Meanwhile, doctors do not recommend simply boosting a person's cortisol levels in an attempt to "fix" the problem.
"There is no evidence that replacing cortisol in someone with long Covid would be a safe or effective thing to do," Sala said.
The study also found that dormant viruses, such as the one that causes mononucleosis, Epstein-Barr, come alive again in long Covid patients. It's unclear, however, whether those old viruses are causing symptoms or flagging a problem within the immune system.
"We were looking for signals, and we found them," said Akiko Iwasaki, one of the researchers and a professor of immunobiology and molecular, cellular and developmental biology at the Yale School of Medicine. "Now what we need to do is home in on each of these signals and understand better how the disease has been driven by these signals."
The investigators did not find significant evidence that long Covid is the result of an autoimmune disorder, in which the body attacks itself.

Joshua Roman practices the cello at his New York City home on Sunday. Long Covid left Roman with uncontrollable trembling, threatening his career.Jonathan Yap
Dr. Clinton Wright, director of the National Institute of Neurological Disorders and Stroke's division of clinical research, said additional studies will be necessary to find other ways Covid may lead to long-term symptoms. One theory is that the virus is hiding in brain tissue or other organs.
"We're really interested in whether the virus still exists in reservoirs in the body," he said. "It's really hard to do that by measuring blood." He was not involved with the new study.
Long Covid affects 1 in 13 U.S. adults, or 7.5%, according to the Centers for Disease Control and Prevention.
The findings offer hope to patients like Joshua Roman, 39, of New York City, who participated in the study.
"We're in such a mysterious swamp of symptoms," he said. "My long Covid treatment is just management of symptoms."
Roman, a professional musician who plays the cello, takes daily medication to ease the lingering physical trembling that affects his ability to perform.
"It would be great if we could get to the thing that's causing me to shake in the first place, but we still don't know exactly what that is," he said















/https://static.texastribune.org/media/files/cc6ae61f5e8226773e87821a82f80e61/1110%20Alice%20Barton%20Portrait%20JS%20TT%2006.jpg)
/https://static.texastribune.org/media/files/303de54aefa3216d08e31b6d82c8ef59/1110%20Abbott%20Vaccine%20Bill%20JS%20TT%2020.jpg)
/https://static.texastribune.org/media/files/289b6347f35213548e845cedb864c3e0/1110%20Alice%20Barton%20Portrait%20JS%20TT%2014.jpg)