In a breakthrough, diabetics’ damaged cells regenerated to produce insulin
Researchers have taken a big step forward in the quest to regenerate the pancreatic beta-cells damaged by type 1 diabetes. Using FDA-approved drugs usually given to patients with rare cancers, they reprogrammed pancreatic cells to produce and secrete insulin in response to glucose. The discovery…
By Paul McClure
January 03, 2024

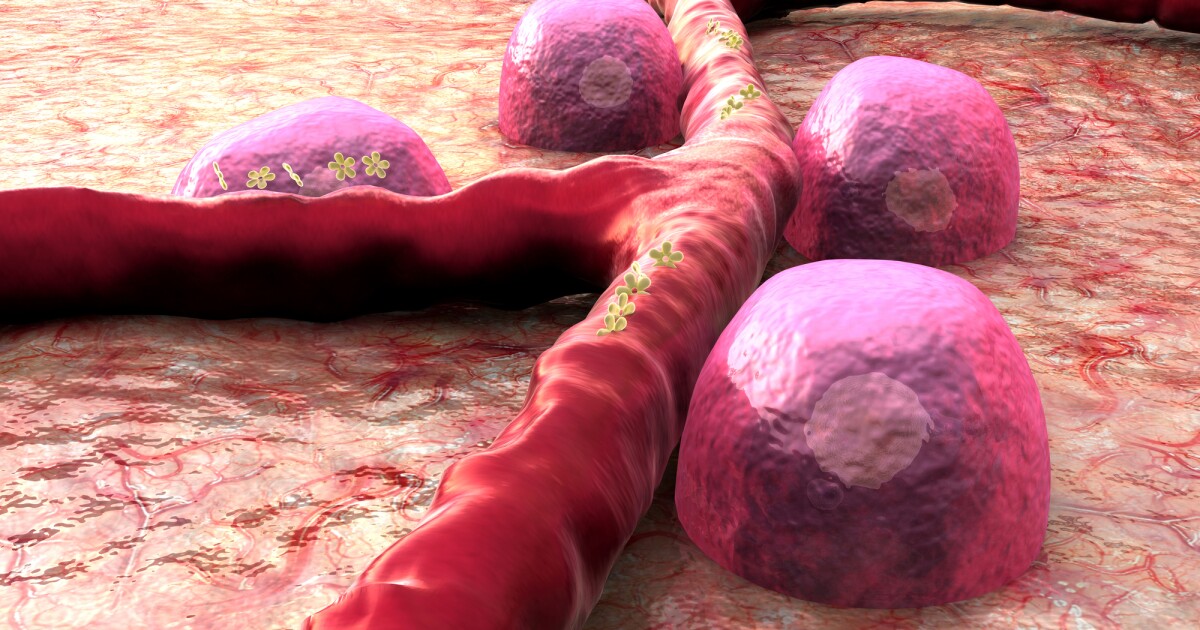
Researchers have regenerated pancreatic cells damaged by diabetes, reprogramming them to produce insulin
Depositphotos
Researchers have taken a big step forward in the quest to regenerate the pancreatic beta-cells damaged by type 1 diabetes. Using FDA-approved drugs usually given to patients with rare cancers, they reprogrammed pancreatic cells to produce and secrete insulin in response to glucose. The discovery could mean that, one day, diabetics won't need to take multiple daily insulin injections.
Pancreatic beta-cells synthesize, store and release insulin. But, in type 1 diabetes (T1D), the immune system selectively destroys these cells over time, leading to a lifelong dependence on exogenous insulin administration for survival. While insulin therapy helps control blood glucose, it doesn’t prevent, stop, or reverse the destruction of the pancreas’ insulin-secreting cells.
For many years, research has focused on identifying novel therapies that stimulate beta-cell growth and function to restore insulin production in type 1 diabetics. Now, in an exciting breakthrough, researchers at the Baker Heart and Diabetes Institute in Melbourne, Australia, have brought us a step closer to making this a reality, regenerating damaged pancreatic cells so they can produce insulin and functionally respond to blood glucose levels.
“We consider this regenerative approach an important advance towards clinical development,” said Sam El-Osta, the study’s corresponding author. “Until now, the regenerative process has been incidental and lacking confirmation; more importantly, the epigenetic mechanisms that govern such regeneration in humans remains poorly understood.”
The study builds upon previous proof-of-concept research by Baker Institute scientists, where they used an EZH2 inhibitor with a naturally derived drug to stimulate ductal progenitor cells, descendants of stem cells, into beta-like cells capable of producing insulin. Ductal cells are exocrine cells that form the lining of the tubes (ducts) that deliver pancreatic enzymes.
Enhancer of zeste homolog 2 (EZH2) is an enzyme that forms part of the protein group polycomb repressive complex 2 (PRC2), which regulates gene expression. EZH2 is also critical in stem cell renewal, maintenance, and differentiation into specific cell lineages. Mutation and overexpression of EZH2 results in the suppression of genes responsible for cell cycle control, leading to uncontrolled growth and cancer. That’s why EZH2 inhibitors are used to treat some cancers.
In the current study, the researchers looked at the ability of two FDA-approved EZH2 inhibitors normally used to treat rare forms of cancer, GSK126 and tazemetostat (Tazverik), to reactivate pancreatic progenitor cells. They obtained pancreatic cells from three donors aged seven, 56 and 61. The seven- and 61-year-olds had T1D; the 56-year-old donor was not diabetic. The seven-year-old donor had only had diabetes for one month, whereas the 61-year-old had had the disease for 33 years.
Inhibiting EZH2 pharmacologically with GSK and tazemetostat caused the pancreatic cells from the juvenile and adult diabetic donors to shift towards a beta-like cell identity. Despite the destruction of pancreatic beta-cells, the researchers found that stimulation of pancreatic ductal cells with GSK126 and tazemetostat could influence insulin (INS) gene expression and was correlated with the expression of maintenance markers that define the beta-cell. After 48 hours of stimulation with the drugs, the reprogrammed cells produced and secreted insulin in response to a physiological glucose challenge.
The novel therapeutic approach has the potential to become the first disease-modifying treatment for T1D, facilitating glucose-responsive insulin production by regenerating the patient’s pancreatic cells. It represents a promising solution for the millions of insulin-dependent diabetics in the world, intending to restore insulin production and free them from multiple daily insulin injections.
The next step is to investigate the therapy in a preclinical model.
The study was published in the journal Signal Transduction and Targeted Therapy.
Source: Baker Heart & Diabetes Institute