The groundbreaking approval has been eagerly anticipated by patients and doctors alike. The treatment is priced at $2.2 million per person.

www.nbcnews.com
FDA approves cure for sickle cell disease, the first treatment to use gene-editing tool CRISPR
The groundbreaking approval has been eagerly anticipated by patients and doctors alike. The treatment is priced at $2.2 million per person.
Dec. 8, 2023, 11:19 AM EST / Updated Dec. 8, 2023, 1:19 PM EST
By
Berkeley Lovelace Jr. and Marina Kopf
The Food and Drug Administration on Friday approved a
powerful treatment for sickle cell disease, a devastating illness that affects more than 100,000 Americans, the majority of whom are Black.
The therapy, called Casgevy, from Vertex Pharmaceuticals and CRISPR Therapeutics, is the first medicine to be approved in the United States that uses the
gene-editing tool CRISPR, which won its inventors the Nobel Prize in chemistry in 2020.
“I think this is a pivotal moment in the field,” said Dr. Alexis Thompson, chief of the division of hematology at Children’s Hospital of Philadelphia, who has previously consulted for Vertex. “It’s been really remarkable how quickly we went from the actual discovery of CRISPR, the awarding of a Nobel Prize, and now actually seeing it being an approved product.”
The approval marks the first of two potential breakthroughs for the inherited blood disorder. The FDA on Friday also approved a second treatment for sickle cell disease, called Lyfgenia, a gene therapy from drugmaker Bluebird Bio. Both treatments work by genetically modifying a patient’s own stem cells.
Until now, the only known cure for sickle cell disease was a bone marrow transplant from a donor, which carries the risk of rejection by the immune system, in addition to the difficult process of finding a matching donor.
Casgevy, which was approved for people ages 12 and older, removes the need for a donor. Using CRISPR, it edits the DNA found in a patient’s stem cells to remove the gene that causes the disease.
“The patient is their own donor,” Thompson said.
“It’s a game-changer,” said Dr. Asmaa Ferdjallah, a pediatric hematologist and bone marrow transplant physician at the Mayo Clinic in Rochester, Minnesota. “To really reimagine and re-discuss sickle cell disease as a curable disease and not as this painful and debilitating chronic disease is hope enough with this news.”
Still, the new therapy is extremely expensive — $2.2 million per patient, Vertex said. The pricing strategy, experts argue, may place it out of reach for many families. What’s more, that price doesn’t include the cost of care associated with the treatment, like a stay in the hospital or chemotherapy.
“We really have to make sure that it is accessible,” said Dr. Rabi Hanna, a pediatric hematologist-oncologist at the Cleveland Clinic who has previously served on the advisory board for Vertex. “This could be an equalizer for people with sickle cell because many patients cannot pursue career options” because of the illness.
“It’s something families have been aware of in the early research stage, and they’ve been very patiently waiting for years,” Ferdjallah said. “It’s been
eagerly awaited by patients and families, but also by providers and physicians.”
How Casgevy works
In patients with sickle cell disease, red blood cells, which are usually disk-shaped, take on a crescent or sickle shape. This change can cause cells to clump together, leading to clots and blockages in the blood vessels, starving tissues of oxygen. Patients can experience
excruciating pain, breathing problems and stroke.
Casgevy works by editing the DNA in a patient’s stem cells — which are responsible for making the body’s blood cells — so that they no longer produce sickle-shaped cells.
While technically a one-time treatment, a number of steps that span months are required before the patient actually gets the modified stem cells. It begins with a series of blood transfusions over three to four months, after which the stem cells are extracted from the patient’s bone marrow and sent off to a lab where they are edited, Hanna said.
Before they can be reinfused into the patient, however, doctors need to make sure no flawed stem cells remain in the body. To do so, chemotherapy is used to destroy the patient’s bone marrow.
Only then can the edited stem cells be reinfused into the patient, followed by another month or two in the hospital to allow the cells to grow and the patient to recover.
Hanna said he’s always “cautious” when telling families and patients about the one-time treatment because they may have unrealistic expectations.
“There are multiple phases of this journey,” he said.
The clinical trial included 46 people in the U.S. and abroad, 30 of whom had at least 18 months of follow-up care after the treatment. Of those, the treatment has been successful in 29.
LaRae Morning, 29, of Phoenix, was among the trial patients whose treatment was successful.
Her doctors did not expect her to live past the age of 11. Her mother lost several jobs when Morning was a child and a teenager because of her frequent hospital visits.
In April 2021, Morning joined the clinical trial at Sarah Cannon Research Institute and HCA Healthcare’s The Children’s Hospital at TriStar Centennial in Nashville, Tennessee, a decision she initially regretted. Living in Phoenix, she had to fly to Nashville once a month for treatment. It included several blood transfusions, which lasted eight hours each, and taking a medication, called plerixafor, which she recalled causing her intense stomachaches. When she started chemotherapy, her hair began to fall out and her skin changed color, resembling the appearance of a chemical burn. She also experienced nausea.
It took about six to seven months for her to feel back to normal following the CRISPR treatment. Now, she said, she’s feeling the benefits, going out to coffee shops, spending time with her friends and finishing her first semester of law school in Washington, D.C.
“Now that I’m here, I’m so happy that I did it,” she said of the trial. “I’m just like a regular person. I wake up and do a 5K. I lift weights. If I wanted to swim, I can swim. I’m still trying to know how far I can stretch it, like what are all the things I can do.”
That’s been the experience for several other patients in the trial as well, according to Dr. Monica Bhatia, chief of pediatric stem cell transplantation at NewYork-Presbyterian/Columbia University Irving Medical Center. Bhatia is a principal investigator at one of the clinical trial sites in New York City.
Following the treatment, most patients were going back to school, going to the gym or resuming other activities — “things that a lot of people take for granted,” she said — after about three to four months.
“They’re really able to live life without restrictions,” Bhatia said.
Dr. Haydar Frangoul, medical director of pediatric hematology-oncology for the Sarah Cannon Research Institute, said he is hopeful the therapy will provide relief to more patients.
“I think this is a huge moment for patients with sickle cell disease,” said Frangoul, who was the lead investigator on the clinical trial and treated Morning.
Long-term questions
Although Casgevy has been shown to be effective, experts still don’t know about potential long-term effects, since the trial is only set to run for two years.
During a meeting in October,
an FDA advisory committee discussed the risk of “off-target” effects, which refers to when the gene-editing tool makes cuts to other stretches of DNA other than the intended target and how the FDA should consider those risks moving forward.
It’s unclear what effects an off-target edit would have on a patient, but the fear is that it could result in unintended health consequences down the road, Thompson said. “To date, there do not appear to be measurable consequences.”
The FDA did, however, add a boxed warning — the strongest safety warning label— to Bluebird Bio’s Lyfgenia, noting that in rare cases the treatment can cause certain blood cancers.
Dr. Nicole Verdun, director of the Office of Therapeutic Products in the FDA's Center for Biologics Evaluation and Research, said Lyfgenia was given the warning after two patients who got the therapy in a clinical trial died from a form of leukemia.
It's unclear whether the gene therapy itself or another part of the treatment process, such as the chemotherapy, caused the cancer, but Verdun said the agency thought the deaths "rose to the level of a black-box warning." No cases were seen in the Vertex clinical trial, she said.
Bhatia is following the patients for 15 years as part of a post-approval study for Casgevy and will be monitoring for signs of long-term effects.
“Long-term follow-up is still going to be so crucial,” she said.
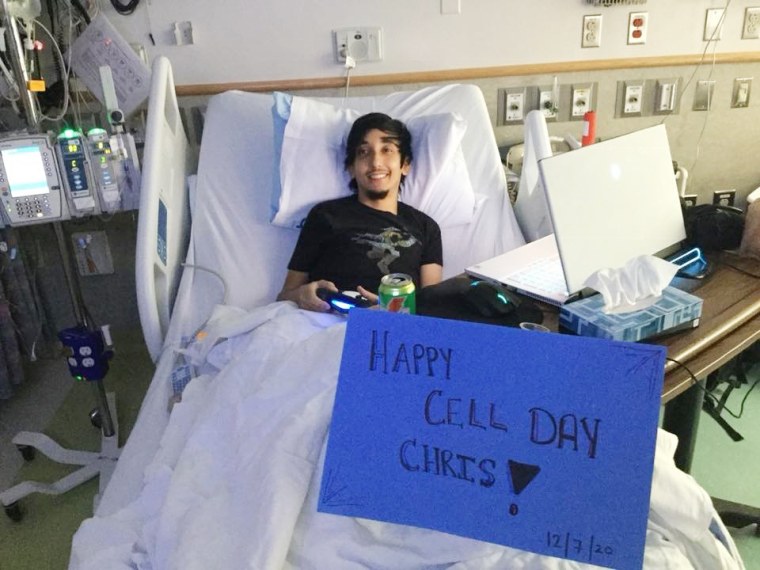
Christopher Vega, 31, of Allentown, Pa., on Dec. 7, 2020, the day he got his infusion of CRISPR-edited stem cells.Courtesy Christopher Vega
Christopher Vega, 31, from Allentown, Pennsylvania, said the possibility of long-term effects aren’t a concern for him; he is happy to be living a life free of chronic pain.
He joined the clinical trial at the Children’s Hospital of Philadelphia in late 2020. He had suffered from chronic fatigue since he was a young child and would end up in the hospital every year with a pain crisis.
“When I was younger, my mom used to always tell me things happen for a reason. And I had so much trouble believing that, because I always thought, ‘Why me?’” he said.
While the treatment process was not always easy — Vega temporarily lost his hair, felt weak and nauseous and developed skin rashes — he said it was worth it.
“I am a whole different person,” said Vega, who is now attending the Los Angeles Film School online for visual effects while taking care of his 5-year-old daughter.
“Sometimes I would get small moments of anxiety that I would have a crisis,” he said. “And after going years now, I’m slowly coming to terms with, I’m OK, and I know I’m going to be here, present.”